Bariatric Surgery
Laparoscopy for a sweet resolution
Diabetes is a global epidemic affecting millions of people across the world, around 347 million people worldwide have diabetes. Diabetes is a global epidemic affecting millions of people across the world, around 347 million people worldwide have diabetes. In 2012 diabetes was the direct cause of 1.5 million deaths. More than 80% of diabetes deaths […]
READ MOREBariatric Surgery | 4 Types of Bariatric Surgery
Bariatric Surgery or Bariatrics is the branch of medicine dealing with the study of obesity, the causes, prevention and treatment of obesity. The Greek word Baro means heavy or large. Diet, exercise, anti-obesity drugs, behavioral therapy are first line treatments of obesity, but success is limited in people with severe obesity. Bariatric Operation or Weight […]
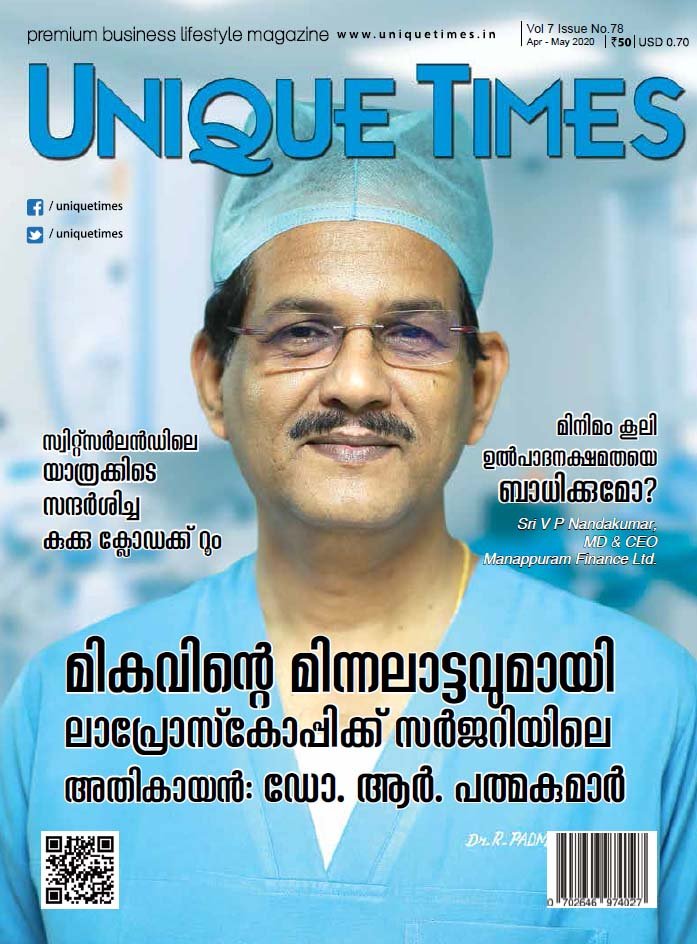
READ MOREWeight Loss Surgery Kochi – VPS Lakeshore Hospital

VPS Lakeshore Hospital is the center for Weight Loss Surgery in Kochi, Kerala headed by Dr. R. Padmakumar. VPS Lakeshore hospital launched Lakeshore Obesity Clinic, a dedicated and comprehensive weight loss clinic. Famous Music Director Deepak Dev, Actress Aparna Balamurali, VPS Lakeshore CEO S K Abdulla and the LOC team together unveiled the LOC logo. […]
READ MOREObesity and Infertility – Does obesity affect pregnancy?
Obesity and Infertility: Obesity is a life-long, progressive, life-threatening, genetically-related, multi-factorial disease of excess fat storage. BMI (Body Mass Index) = Weight in Kg / Height in M2. For Asian populations, classifications remain the same as the international classification, but public health action points for interventions are set at 23, 27.5, 32.5 and 37.517. Obesity […]
READ MOREWeight Loss Treatment – Newer Modalities of Treatment for Obesity
Weight Loss Treatment : It will be a wish of everybody to have an attractive body figure. There was a time when majority were running around to find ways to increase body weight but today great majority are depending on various methods and advertisements modalities for reducing body weight. It is very happy to know […]
READ MOREIntragastric Balloon or Gastric Balloon Placement for Weight Loss
Intragastric Balloon Placement is placing a deflated balloon in the stomach using endoscopy and then filling it to decrease the amount of intragastric space. It can be left in the stomach for a period of 6 months and results in average weight loss of 10-15 kg in half a year. It may be used in […]
READ MOREBypass Procedures for Weight Loss
These are malabsorptive procedures. In this the stomach is connected to a distal part of the intestine so that the absorption is reduced and thus causing weight reduction. There is good weight loss and resolution of metabolic syndrome to great extent. It is less preferred due to shunting of food (dumping syndrome) and some vitamin […]
READ MORELaparoscopic Sleeve Gastrectomy for Weight Loss (> 30 BMI Patients)

Laparoscopic Sleeve Gastrectomy is a surgical procedure for weight loss. In this procedure, the stomach is reduced to about 15% of the original size of the stomach by removing a large portion of the stomach along the greater curvature. The portions of stomach which secretes Ghrelin (hormone which increase appetite and cholesterol) and acid (which […]
READ MORE

-
Anal Fissure Treatment
- Piles / Hemorrhoids Treatment
- Varicose Veins Treatment
- Laser Treatment for Varicose Veins
- Diabetic Foot Treatment
- Gynaecomastia