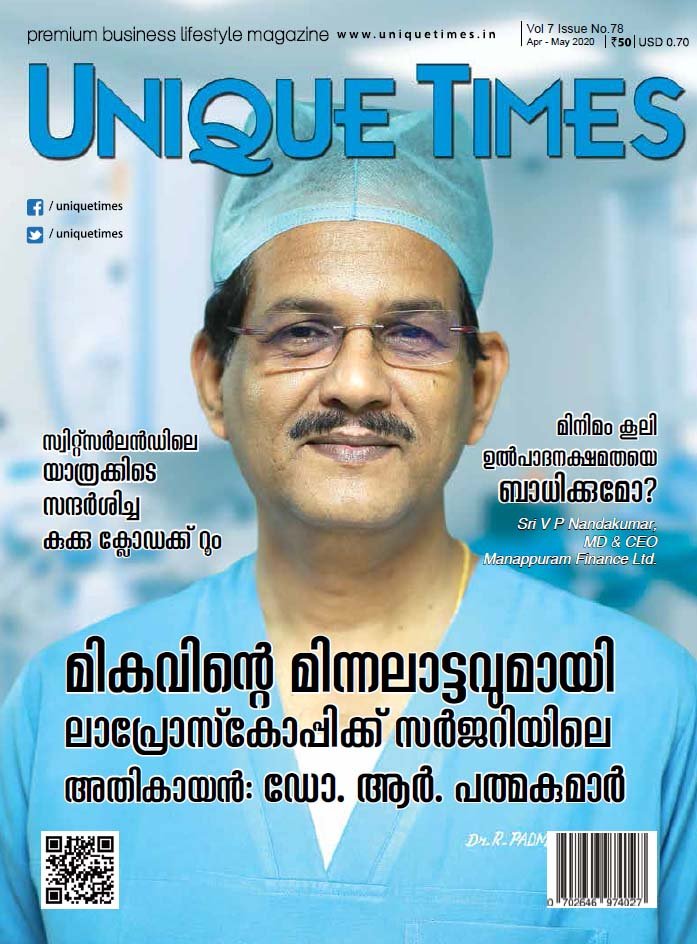
Laparoscopic Hernia Repair
TAPP INGUINAL HERNIA REPAIR
TAPP Inguinal Hernia Repair Patient Selection for TAPP Inguinal Hernia Repair Difficult cases: Direct or small indirect primary hernias in lean and thin subjects are the best during learning curve. Anesthesia General anesthesia Skin Preparation No studies are there assessing preparation for hernia surgery, but as with other surgical procedures, there is no difference in […]
READ MOREInguinal Anatomy with Peritoneum Incised
Previous Page – Inguinal Anatomy with Peritoneum Intact After the peritoneum is dissected away, six additional structures need to be identified. They are Pubic Crest: It helps in getting orientation. Beware of small veins overlying. If they bleed entire vision gets spoiled. Iliopubic Tract: The iliopubic tract is a thick fibrous white tract which runs […]
READ MOREInguinal Anatomy with Peritoneum Intact
Anatomy of Inguinal Region – Previous Page With the introduction of the laparoscope into the abdomen, five important landmarks can be identified in the infra-umbilical region. Inferior epigastric vessels Medial umbilical ligament Spermatic vessels Vas deferens Trapezoid of disaster Inguinal Anatomy with Peritoneum Intact Inferior epigastric vessels The inferior epigastric artery is prominently visualized during […]
READ MOREInguinal Region – Anatomy, Part 2
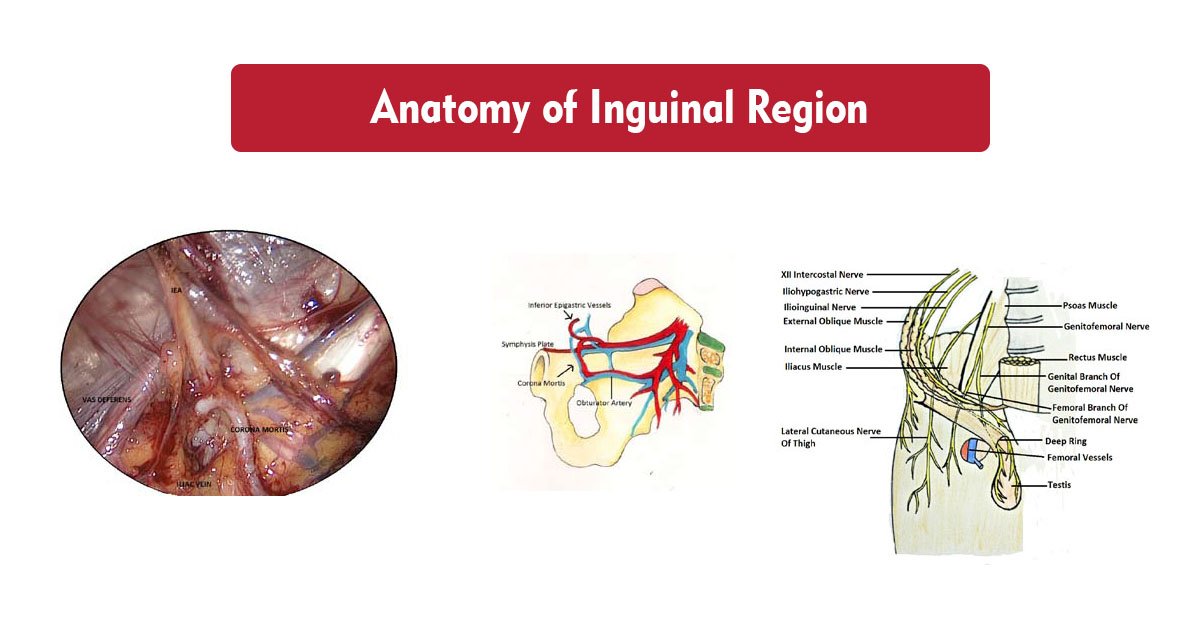
Anatomy of Inguinal Region – Previous Page Transversalis Fascia (of Gallaudet) This fascia is a two layered structure (bilaminar). The anterior layer is adherent to the rectus abdominis muscle. The posterior layer lies in between the anterior layer and the peritoneum. It divides this space into an anterior (vascular space) and a posterior (Space of […]
READ MOREInguinal Region – Anatomy, Peritoneal Landmarks, Infraumbilical Fossae – Part 1
Anatomy of the Inguinal Region The ‘Myopectineal Orifice of Fruchaud’ All groin (inguinofemoral) hernias originate in a single weak area called the myopectineal orifice. This oval, funnel-like, ‘potential’ orifice formed by the following structures, makes the ‘myopectineal orifice of Fruchaud’.-Henry Fruchaud Boundaries Superiorly Internal oblique and transversus abdominis muscles. Inferiorly Superior pubic ramus. Medially Rectus […]
READ MOREAdvantages of Laparoscopic Hernia Repair and Difficulties
Advantages Laparoscopic Hernia Repair Level 1A evidence Lower incidence of wound infection and hematoma formation. Lesser pain & discomfort. Immediate postoperative pain and delayed pain is reduced. Shorter hospital stay. Early resumption of normal daily activities and work. Level 1B evidence Incidence of recurrence as low as with Lichtenstein’s repair. Cost-effective when QALY (quality-adjusted life-year) […]
READ MOREIntroduction to Hernia
Repair of inguinal hernia is one of the commonest surgical procedures performed worldwide. The lifetime risk for men is 27% and for women, it is 3 %. “No disease of the human body, belonging to the province of the surgeon, requires in its treatment, a better combination of accurate, anatomical knowledge with surgical skill than […]
READ MORELaparoscopic Hernia Repair

Laparoscopic Hernia Repair – How to Learn at Ease By Dr. R. Padmakumar and Dr. Madhukar Pai & Dr. Farish Shams Section 1 INTRODUCTION TO HERNIA Introduction Read More History of hernia repair Read More The Laparoscopic Hernia Repair Advantages & Difficulties Read More Section 2 ANATOMY LAPAROSCOPIC VIEW – Anatomy of the Inguinal Region […]
READ MORE

-
Anal Fissure Treatment
- Piles / Hemorrhoids Treatment
- Varicose Veins Treatment
- Laser Treatment for Varicose Veins
- Diabetic Foot Treatment
- Gynaecomastia